Drexel University and Pace Surgical, Inc. develop biointegrative suture anchor
Nathan Snizaski
Feb 26, 2025
Soft tissue tears are among the most common injuries, and many require surgical repair using tiny devices called suture anchors. Traditional anchors can sometimes fail when attached to low-density bone, making repairs more complicated. To address this challenge, a team of researchers at Drexel University partnered with Pace Surgical, Inc. (Philadelphia, PA) to develop a new class of suture anchors that expand naturally by absorbing body fluids, achieving superior fixation compared to conventional anchors.
Torn muscle tissue can result from a traumatic event, such as a sports injury, or from repeated activity. After the tissue tears from the bone, it needs to be surgically reattached to the bone. The most common method involves placing an anchor—typically a metal screw—into the bone and then reattaching the soft tissue using a suture, which reattaches the tissue back to the bone.
With low bone density, the anchor for the suture may pull out, resulting in serious complications. The Drexel research team partnered with Pace Surgical to investigate a viable and superior alternative to conventional sutures, based on a different mechanism that supports anchoring for patients with low bone density.
“The current state of the art for sutures uses screws that serve as anchors,” says Sorin Siegler, professor emeritus at Drexel University’s College of Engineering. “In low-density bone—such as people with osteoporosis—the screws tend to pull out, particularly in the shoulder, where the bone is weak to begin with. Rotator cuff repairs are notoriously difficult to use suture anchors.”
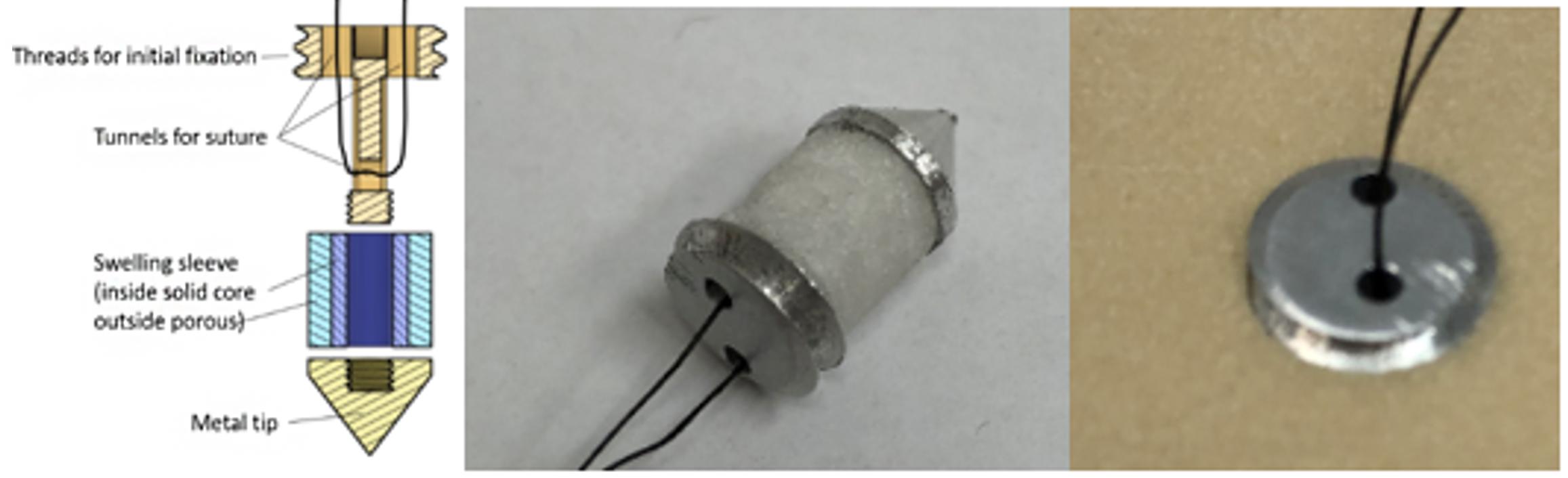
Instead of relying solely on screw threads, the research team explored ways to create an anchor that swells against the bone, maximizing fixation strength. Siegler conceived the idea for the swelling technology from drywall screws.
“Let’s say you want to hang a picture in your home,” he explains. “You could drill a metal screw into drywall and hope that the screw supports the weight of the picture. However, drywall is very weak with very low density. The screw threads will shear very quickly, and the whole screw tears or pulls out from the drywall threads rather easily.”
To prevent the shearing effect of the screw, the research team developed a biointegrative material made from two monomers. When mixed with a catalyst, the liquid solidifies into a copolymer that can absorb interstitial fluid—fluid found in the spaces around cells in the body.
“What’s unique about this approach is the relationship between the two monomers,” says Siegler. “One is hydrophilic and likes water, while the other is hydrophobic and doesn’t like water. By combining them in the right amounts, you get a material that is solid yet swells by a controlled amount. We can design it to swell by whatever amount we want to adapt it to the surrounding bone.”
Unlike conventional anchors, the swelling caused by the copolymer device will stimulate osteointegration. As the copolymer device swells, the surrounding bone densifies to create an integrated fixation.
“Bones are a living tissue,” says Siegler. “Wolff’s Law (named after the German surgeon and anatomist Julius Wolff) basically states that when stressors are acting on the bone, it responds by growing. If you remove that stress, it starts to resorb and go away. We want to leverage this law by inducing a positive form of stress on the bone to support long-term surgical fixation.”
Our research has an opportunity to provide superior fixation of a suture anchor due to its expansion mechanism.
Sorin Siegler, professor emeritus, Drexel University
Early studies suggest that the swelling material not only offers strong fixation and integration with bone tissue, but also reduces damage during anchor pullout and may even promote bone strengthening around the implant.
Siegler credits Pace Surgical’s CEO, Jeffrey F. O’Donnell, Jr., and CTO, Bill Rhoda, for their expertise in orthopedics, which helped shape the prototype design. He also acknowledges the Manufacturing PA Innovation Program’s role in supporting the project’s transition from research toward productization.
“The support we received from the program enabled us to advance to the next step. It came at just the right time to facilitate the direction of commercialization.”
The research team continues to test prototypes developed through the collaboration, with the ultimate goal of advancing the technology into clinical use as a device for orthopedic surgeons.
“Fixation to bone is the number one requirement in orthopedic surgery,” says Siegler. “We’re targeting the rotator cuff as the first application because rotator cuff sutures tend to fail at an unacceptable rate. If we manage to penetrate the market for rotator cuff surgeries, then I believe there will be no limit in getting into many other applications where fixation to bone is required.”